Oct 24 2024 43 mins 13
We are joined today by two amazing educators from NYU for our latest Fellows’ Case Files Episode. Listen today as we go through a great case with some fantastic teaching points highlighted throughout the episode.
Meet Our Guests
Dr. Jeremy Grossman completed his Medicine-Pediatrics residency at Stony Brook Medicine where he was also a Chief Resident. He is currently a second-year PCCM fellow at NYU.
Dr. Shari Brosnahan is an Assistant Professor of Medicine and one of the Assistant Program Directors for the NYU Langone’s Division of Pulmonary, Critical Care, and Sleep Medicine. Her clinical and research interests are focused on pulmonary embolism and thrombosis in critically ill patients.
Case Presentation
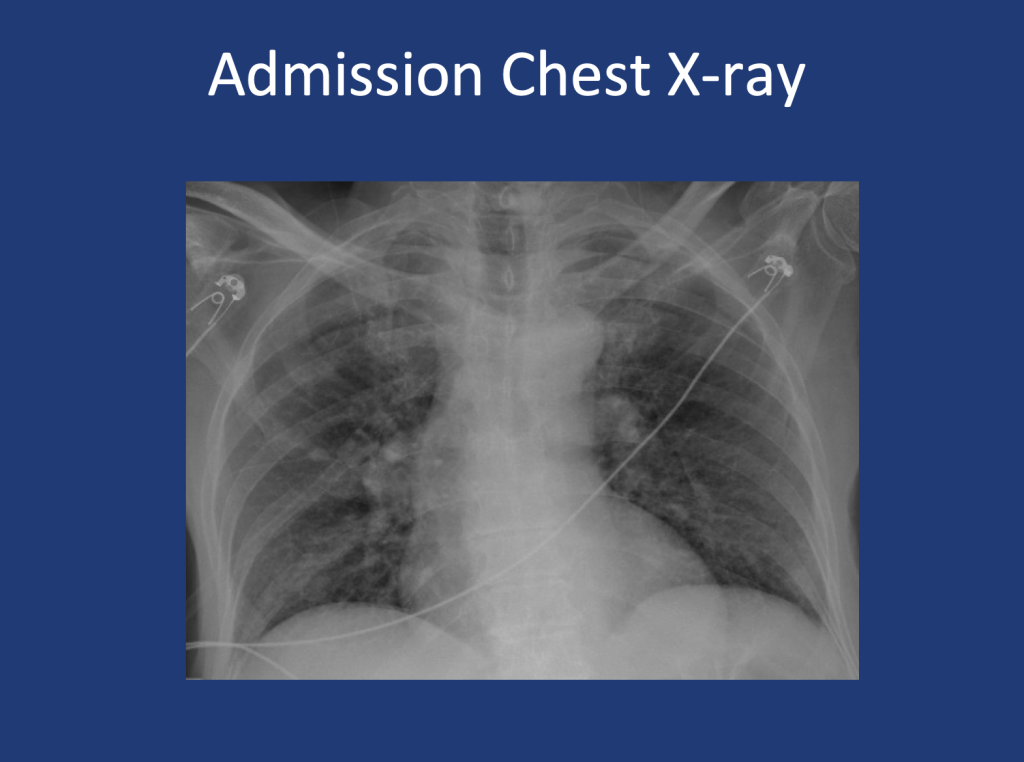
An 80-year-old male presents with shortness of breath. At home, his oxygen saturation was 82% on room air, improving only to 86% on 4L nasal cannula. Over the past month, he has experienced worsening symptoms, including a dry cough, fatigue, and difficulty speaking or ambulating due to shortness of breath at rest. He denies recent fever, sputum production, chest pain, or lower extremity swelling and presents to the ED for further evaluation.
Key Learning Points
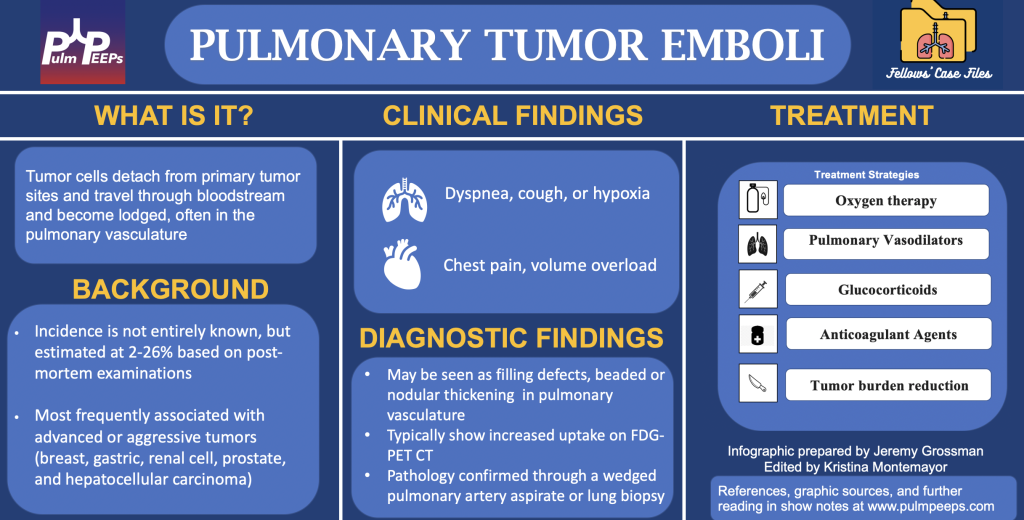
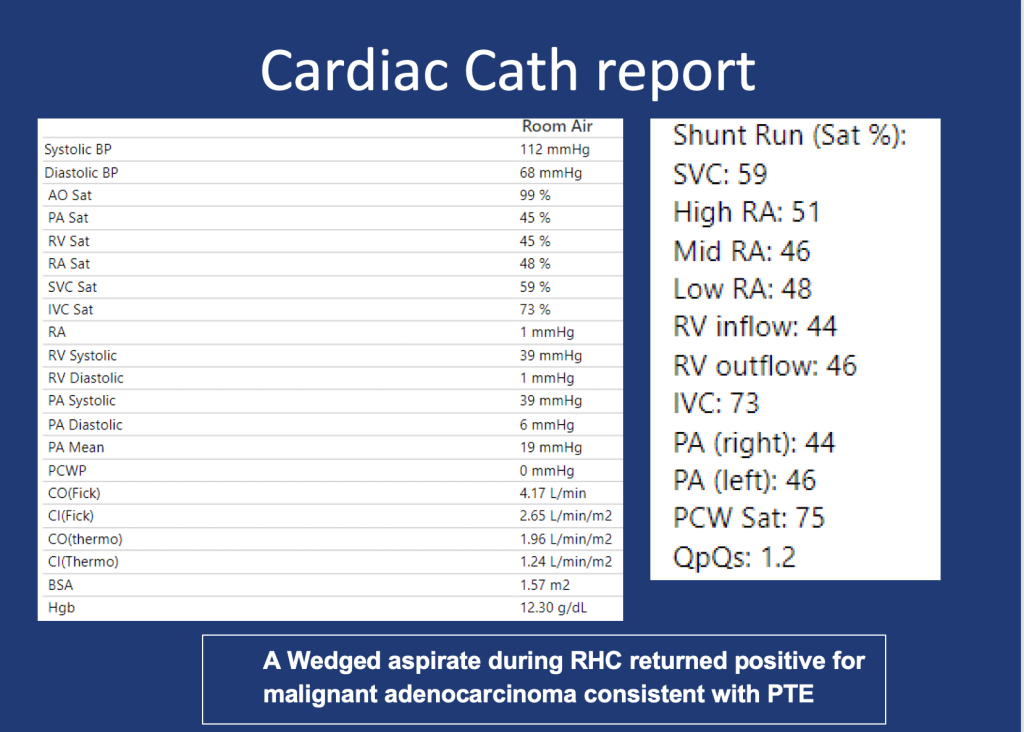
1.In any patient with a history of malignancy and hypoxia, clinicians should keep pulmonary tumor emboli (PTE) on the differential as early intervention may alter outcomes.
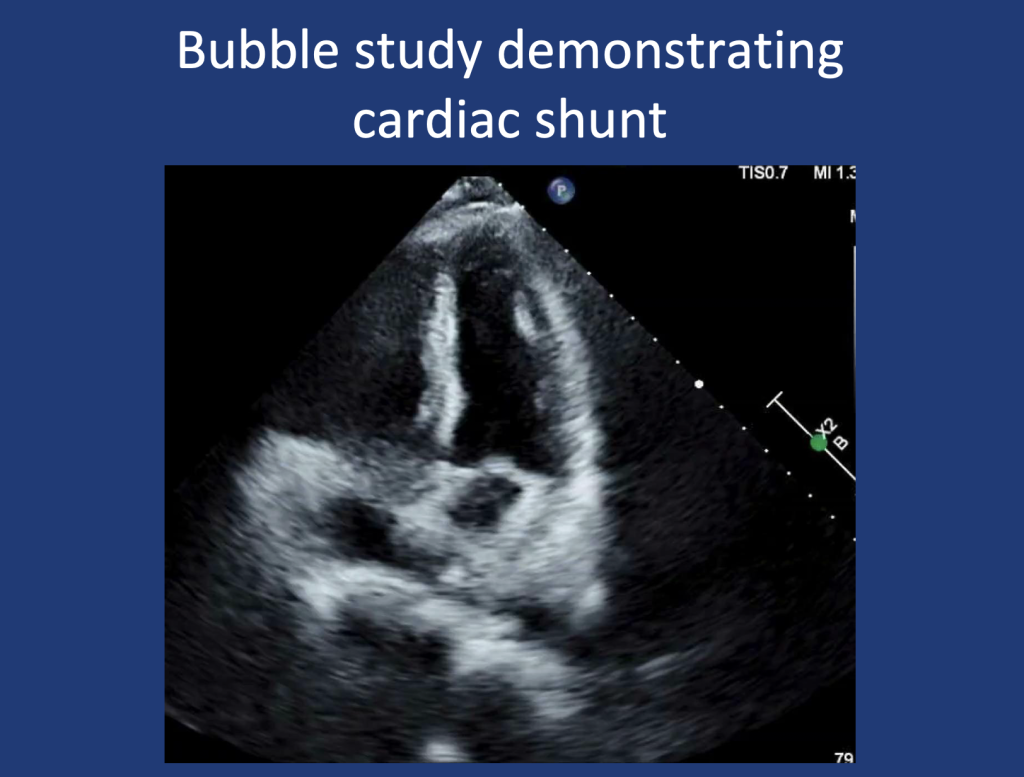
2.PTE contributes to hypoxia via mechanisms of mechanical obstruction of pulmonary arteries leading to shunting, VQ Mismatch, and in some cases pulmonary hypertension due to increased PVR.
3.A wedged aspirate can be used to diagnose PTE ante-mortem